
More than 2.8 million lives covered by Delta Dental of Ohio
Thank you for your continued dedication to our members!
For the record
How do Ohioans stack up against the nation when it comes to dental benefits? Consider these facts from the National Association of Dental Plans.
- An estimated 81 percent of the Michigan population has dental benefits, compared to 80 percent of the national population.
- Of those with dental benefits nationwide, 89.6 percent receive benefits through a large group plan.
- The number of adults nationwide who had a dental check-up in the last 12 months included:
- 61 percent with dental benefits
- 37 percent without dental benefits
Back to top
Customer service and operations corner
There are a few things you can do to help speed up your claim submission timeline. Here are a few tips:
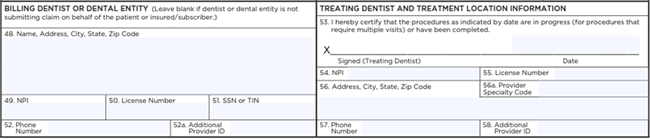
- The most preferred claim form is the ADA standard dental claim form.
- The “Billing Dentist” and “Treating Dentist” fields are some of the most important fields to be completed.
- When submitting a claim, ensure you’ve completely filled out the “Billing Dentist or Dental Entity” boxes (48–52) and the “Treating Dentist and Treatment Location Information” boxes (53–57).
Back to top
A partner in Medicare Advantage
Earlier this year, Delta Dental Insurance Company and Devoted Health’s Medicare Advantage plan partnered to provide dental services to thousands of members nationally, including members in Ohio.
Eligible members will use the Delta Dental of Ohio Medicare Advantage™ PPO network when seeking an in-network provider. If you participate in the Delta Dental PPO™ network you are also participating in the Medicare Advantage PPO network. When providing non-covered treatment to a Delta Dental Medicare Advantage patient, please remember to have the patient sign a private pay form, which includes the date of treatment, the procedure code(s) and the fees. You can create your own form or feel free to use our sample form.
Provider offices can call 855-251-9742 or visit the Provider Tools Portal for Devoted plan confirmation and member benefits at www1.deltadentalins.com/dentists/provider-tools.html.
When submitting a claim for Devoted members, send it to:
Delta Dental Claims Department
Delta Dental Insurance Company
PO Box 1809
Alpharetta, GA 30023
Back to top
New options added to CE
course lineup

The list of CE courses Delta Dental provides at no cost for participating providers and their staff is growing!
Ethics and Jurisprudence was added in July, and covers dental ethics, professional definitions (RDA, RDH, dental therapist, dentist, specialist), delegation, supervision, assignment, dental record requirements and jurisprudence.
- Course participants will learn the rules regarding assignment of duties to various dental professionals and staff, the standards of record keeping according to the ADA and various aspects of jurisprudence.
- One CE credit can be earned by completing this course.
- While the content only applies to Michigan providers, those in Ohio and Indiana are invited to participate.
Infection Control was added earlier this year and reviews CDC guidelines on infection control in the dental office.
- Course participants will review CDC guidelines on infection control in the dental office, while also reviewing hand hygiene, PPE, respiratory hygiene, sharps safety, injection safety, sterilization, environmental safety, waterline safety and program development.
- One CE credit can be earned by completing this course.
Visit www.deltadentaloh.com/onlineeducation for a full course list and more details.
Delta Dental Plan of Michigan Inc. is an ADA CERP-recognized provider.
Back to top
Participating in the MA network
When you sign on to participate in the Delta Dental PPO™, Delta Dental Premier® or Delta Dental EPO™ networks, you get one more advantage—automatic participation in the corresponding Delta Dental Medicare Advantage™ network.
You will be listed in the Medicare Advantage dentist search for those members, and services rendered are on the same fee schedule as the primary network you signed on to, whether that is Delta Dental PPO, Delta Dental Premier or Delta Dental EPO. The only difference when treating patients with Medicare Advantage versus a commercial plan is that you need to fill out a private pay form before providing any non-covered services.
You can create your own form or feel free to use our sample form. The patient must sign the form and your office should include it as part of the patient record.
Participating dentists should reference their Delta Dental agreement about any charges for non-covered services provided to Medicare Advantage members or those with Medicaid benefits.
Back to top
Removing barriers to care
The leading unmet health care need for millions of U.S. children and adults with a disability is adequate dental care. Delta Dental’s Special Health Care Needs Benefit reduces barriers to care by providing eligible members with enhanced benefits.
If you have a member with this benefit as part of their plan, they may receive:
- Additional visits to the dentist’s office and/or consultations that can be helpful prior to the first treatment to help them learn what to expect and what is needed for a successful dental appointment. Additional exam benefits will be allowed for this purpose.
- Up to four total dental cleanings in a benefit year.
- Treatment delivery modifications, including anesthesia and nitrous oxide, necessary for dental staff to provide oral health care for those with sensory sensitivities, behavioral challenges, severe anxiety or other barriers to treatment.
Before rendering services, check the member’s procedure eligibility in the Dental Office Toolkit® (DOT). If the member’s record has been updated to allow for additional services under this benefit, there will be a message in DOT confirming this.
- If there is not already a message but the member says their Delta Dental plan includes the Special Health Care Needs Benefit and they have a qualifying special health care need, you should include code D9997 on the initial claim submission for the patient.
- After this first claim processes, the member’s procedure eligibility will update accordingly.
Note: There is no age limit on these benefits. When looking in DOT, the “Special Health Care Needs Benefit” message is different from the “Handicap” attribute.
Back to top